The intersection of gynecology and mental health: addressing the psychological dimensions of women's health
La intersección de la ginecología y la salud mental: abordaje de las dimensiones psicológicas de la salud de la mujer
Kirolos Eskandar 1*, https://orcid.org/0000-0003-0085-3284
1 Diakonie Klinik Mosbach. Germany.
* Corresponding author: kiroloss.eskandar@gmail.com
Received: 09/10/2024
Accepted: 10/12/2024
How to cite this article: Eskandar K. The intersection of gynecology and mental health: addressing the psychological dimensions of women's health. MedEst. [Internet]. 2025 [cited access date]; 5(1):e278. Available in: https://revmedest.sld.cu/index.php/medest/article/view/278
ABSTRACT
Introduction: the intersection between gynecology and mental health is a crucial, yet often underappreciated, aspect of women's healthcare. Various gynecologic conditions and treatments have significant psychological implications, highlighting the need to integrate mental health into gynecologic care.
Objective: to explore the psychological dimensions of gynecologic health.
Methods: a systematic review of relevant literature was conducted using databases including PubMed, Google Scholar, Scopus, and Web of Science. Specific keywords, including “Gynecology,” “Mental Health,” and “Holistic Approach,” were used to identify studies on the psychological dimensions of women's health. After a rigorous screening process, 38 articles that met the inclusion criteria were included, providing a comprehensive analysis of the psychological aspects of gynecologic health.
Conclusions: the review highlights the profound impact of hormonal influences, reproductive challenges, and gynecologic cancers on mental well-being, demonstrating the need for holistic care in gynecology. Cultural and socioeconomic factors also influence access to mental health support, reinforcing the need to integrate mental health into gynecologic care. Recommendations include expanding mental health screening and promoting a multidisciplinary approach to improve outcomes and address the unique health care needs of women.
Keywords: Gynecology; Holistic care; Mental health; Psychological well-being; Reproductive health; Women's health
RESUMEN
Introducción: la intersección entre ginecología y salud mental es un aspecto crucial, aunque a menudo subestimado, de la atención sanitaria para mujeres. Diversas afecciones y tratamientos ginecológicos tienen implicaciones psicológicas significativas, lo que destaca la necesidad de integrar la salud mental en la atención ginecológica.
Objetivo: explorar las dimensiones psicológicas de la salud ginecológica.
Métodos: se realizó una revisión sistemática de la literatura relevante utilizando bases de datos como PubMed, Google Scholar, Scopus y Web of Science. Se emplearon palabras clave específicas, como “Ginecología,” “Salud Mental,” y “Enfoque Holístico,” para identificar estudios sobre las dimensiones psicológicas de la salud femenina. Después de un riguroso proceso de selección, se incluyeron 38 artículos que cumplían los criterios de inclusión, proporcionando un análisis exhaustivo de los aspectos psicológicos de la salud ginecológica.
Conclusiones: la revisión resalta el profundo impacto de las influencias hormonales, los desafíos reproductivos y los cánceres ginecológicos en el bienestar mental, demostrando la necesidad de una atención holística en ginecología. Los factores culturales y socioeconómicos también influyen en el acceso a apoyo en salud mental, reforzando la necesidad de integrar la salud mental en la atención ginecológica. Las recomendaciones incluyen la ampliación de los exámenes de salud mental y el fomento de un enfoque multidisciplinario para mejorar los resultados y abordar las necesidades únicas en la atención de salud de las mujeres.
Palabras clave: Atención holística; Bienestar psicológico; Ginecología; Salud mental; Salud reproductiva; Salud de la mujer
INTRODUCTION
The intricate relationship between gynecology and mental health represents a critical facet of women's healthcare that has garnered increasing attention in recent years. Women's reproductive health is profoundly interconnected with their psychological well-being, as hormonal changes, gynecological conditions, and reproductive events can significantly impact mental health. This literature review explores the multifaceted nature of this intersection, emphasizing the necessity for an integrated approach to women's healthcare that addresses both physical and psychological dimensions.
Gynecological health encompasses a range of conditions and life stages, from menstruation to menopause, each of which can influence a woman's mental state. Hormonal fluctuations associated with the menstrual cycle, pregnancy, and menopause can precipitate or exacerbate mental health issues such as depression, anxiety, and mood disorders. (1) For instance, premenstrual dysphoric disorder (PMDD) is a severe form of premenstrual syndrome that includes significant mood disturbances and can profoundly affect a woman's quality of life. (2)
The psychological impact of gynecological conditions like polycystic ovary syndrome (PCOS), endometriosis, and chronic pelvic pain is equally profound. Women with these conditions often experience higher rates of anxiety, depression, and diminished quality of life compared to their healthy counterparts. (3) For example, the chronic pain associated with endometriosis not only affects physical health but also leads to significant emotional distress and psychological burden. (4)
Reproductive events such as pregnancy, childbirth, and the postpartum period are also critical junctures where mental health considerations are paramount. Postpartum depression affects approximately 10-15 % of new mothers, with potential long-term consequences for both the mother and child. (5) The psychological ramifications of infertility and the emotional toll of fertility treatments further underscore the need for mental health support in gynecological care. (6)
Moreover, the mental health of women undergoing treatment for gynecologic cancers is a significant concern. The diagnosis and treatment of cancers such as ovarian, cervical, and uterine cancer can lead to anxiety, depression, and a range of other psychological challenges. (7) Integrating mental health support into oncology care can improve the overall well-being and quality of life for these patients. (8)
Sexual health, a vital component of gynecological care, is closely linked to psychological well-being. Conditions such as sexual dysfunction, vaginismus, and dyspareunia not only affect physical health but also have profound psychological impacts, contributing to distress, relationship difficulties, and decreased quality of life. (9)
Addressing the psychological dimensions of gynecological health requires a multidisciplinary approach that includes mental health screening, patient education, and integrated care pathways. Healthcare providers must be trained to recognize and address mental health issues in their patients, ensuring that comprehensive care includes both physical and psychological aspects. (10) This holistic approach is essential for improving health outcomes and enhancing the overall well-being of women.
The objective of this literature review is to examine the psychological dimensions of gynecological health, focusing on how an integrated approach can improve care quality by addressing both the physical and mental health needs of women across various life stages and health conditions.
METHODOLOGY
A systematic approach was utilized for this literature review, adhering to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to gather relevant articles and studies in Emergency medicine’s critical cases. A thorough search was conducted in reputable databases, including PubMed, Google Scholar, Scopus, and Web of Science, using specific keywords such as “Gynecology”; “Holistic care”; “Mental health”; “Psychological well-being”; “Reproductive health” and Women's health to ensure comprehensive coverage of pertinent literature.
The inclusion criteria for the studies were as follows: publications in English, studies focusing specifically on gynecology and mental health, and studies reporting on psychological dimensions of women's health. Initially, 136 articles were retrieved from the databases. After a meticulous examination to eliminate duplicate references, 38 unique articles met the inclusion criteria. These articles underwent rigorous evaluation through a comprehensive assessment of their titles, abstracts, and full texts, confirming their alignment with the established inclusion criteria and warranting their inclusion in the review.
To provide a clear overview of the study selection process, the PRISMA flow diagram is included below (fig. 1), illustrating the number of records identified, screened, and included in the review, along with reasons for exclusion at each stage.
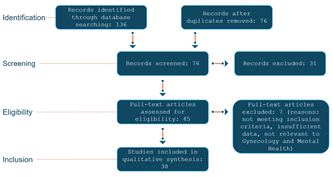
Figure 1: Ilustrates the PRIMSA flow diagram
DEVELOPMENT
Historical Context
The integration of mental health into gynecological care has a profound historical context that reflects the evolving understanding of women's health. Initially, gynecology was predominantly focused on the biological and reproductive aspects of women’s health, often neglecting the psychological dimensions. This limited approach overlooked the significant impact that mental health has on overall well-being and the outcomes of gynecological treatments. Over the past few decades, there has been a growing recognition of the necessity to address mental health within the realm of gynecology, leading to more holistic care models.
The evolution of understanding women’s mental health in gynecology can be traced back to the broader medical field’s increasing acknowledgment of mental health's role in physical health. Historically, conditions like postpartum depression and premenstrual dysphoric disorder were often misunderstood or ignored. However, the late 20th and early 21st centuries saw a paradigm shift, driven by both scientific advancements and advocacy for women’s health rights. Research began to underscore the high prevalence of mental health issues among women experiencing gynecological conditions, highlighting the need for integrated care approaches. (11, 12)
One of the key milestones in this integration was the establishment of interdisciplinary approaches that combine gynecological and psychiatric care. These approaches have proven essential in managing conditions such as endometriosis, polycystic ovary syndrome (PCOS), and menopause, which are often accompanied by significant psychological distress. The recognition of the bidirectional relationship between mental and physical health has been crucial. For instance, stress and anxiety can exacerbate symptoms of gynecological conditions, while chronic gynecological issues can lead to mental health problems. (13)
Moreover, policy changes and advocacy have played significant roles in integrating mental health into gynecological care. Initiatives aimed at training gynecologists to screen for mental health issues and refer patients to appropriate mental health services have been pivotal. Programs emphasizing the importance of mental health screening during routine gynecological visits have also emerged, reinforcing the idea that mental health is integral to overall health.
Additionally, the COVID-19 pandemic has further highlighted the necessity of addressing mental health within gynecology. The pandemic's psychological toll, particularly on women, emphasized the need for comprehensive care models that consider both physical and mental health. Studies have shown that women with pre-existing gynecological conditions experienced heightened levels of anxiety and depression during the pandemic, reinforcing the need for integrated care. (14)
I. Hormonal Influences on Mental Health
Hormonal fluctuations have a profound impact on women's mental health, influencing mood and psychological well-being at various stages of their reproductive lives. The menstrual cycle, hormonal contraception, and menopause are three critical areas where these effects are particularly evident.
The menstrual cycle is characterized by cyclical changes in hormone levels, primarily estrogen and progesterone, which can significantly influence mood and emotional stability. Many women experience premenstrual syndrome (PMS) or the more severe premenstrual dysphoric disorder (PMDD), which are linked to the luteal phase of the cycle when progesterone peaks and then drops sharply. PMS and PMDD symptoms include mood swings, irritability, depression, and anxiety. Research suggests that these symptoms are partly due to the interaction between ovarian hormones and neurotransmitters such as serotonin, which regulate mood. (15)
Hormonal contraception, particularly combined oral contraceptives, can also impact mental health. These contraceptives alter the natural hormonal cycle, leading to a more stable hormonal environment, which can be beneficial for some women but may cause mood changes in others. The impact of hormonal contraception on mental health varies widely among individuals. Some women report improved mood stability, while others may experience increased anxiety or depression. Studies indicate that hormonal contraceptives can influence mood by affecting neurotransmitter pathways and inflammatory markers. (16, 17)
Menopause marks another significant hormonal transition, characterized by a decline in estrogen and progesterone levels. This transition can lead to various psychological symptoms, including depression, anxiety, and mood swings. The menopausal transition can also exacerbate existing mental health conditions. Hormone replacement therapy (HRT) is often used to manage severe symptoms, and research shows it can have beneficial effects on mood and cognitive function, although it is not without risks and must be tailored to the individual. (18)
The interplay between hormonal changes and mental health highlights the need for a comprehensive approach to women's healthcare that integrates both gynecological and psychological perspectives. Addressing these hormonal influences through a combination of medical, psychological, and lifestyle interventions can significantly enhance the overall well-being of women across different life stages.
II. Psychological aspects of gynecological conditions
Gynecological conditions such as endometriosis, polycystic ovary syndrome (PCOS), and fibroids have significant psychological impacts on affected women. Endometriosis, characterized by the presence of endometrial tissue outside the uterus, causes chronic pain and infertility, which often leads to anxiety, depression, and reduced quality of life. (19) Similarly, PCOS, which is associated with hormonal imbalances, irregular periods, and infertility, often results in body image issues, anxiety, and depression. The chronic nature of these conditions exacerbates mental health issues, necessitating comprehensive care that addresses both physical and psychological aspects. (20)
Fibroids, non-cancerous growths in the uterus, can cause heavy menstrual bleeding, pain, and reproductive issues, significantly impacting a woman's mental health. Studies indicate that women with fibroids experience higher levels of stress, anxiety, and depression compared to those without these conditions. (21) The physical symptoms of these gynecological conditions, coupled with their impact on fertility and daily functioning, contribute to significant psychological distress.
Chronic pelvic pain, often associated with these conditions, further complicates mental health. Persistent pain can lead to a cycle of physical discomfort and psychological distress, where each exacerbates the other. Women experiencing chronic pelvic pain frequently report feelings of hopelessness, frustration, and a sense of loss of control over their lives. The pain's chronic nature can lead to sleep disturbances, decreased social interaction, and an overall reduction in quality of life, highlighting the need for integrated treatment approaches that address both pain management and mental health support. (22)
Understanding the psychological dimensions of gynecological conditions is crucial for providing holistic care. Healthcare providers must be aware of the mental health impacts and incorporate psychological assessments and interventions into their treatment plans. This comprehensive approach can help mitigate the mental health burden associated with these chronic conditions, improving overall outcomes for women.
III. Reproductive health and mental well-being
The psychological impact of reproductive health issues such as infertility, pregnancy, and postpartum experiences is profound and multifaceted. Infertility and the use of assisted reproductive technologies (ART) can significantly affect mental well-being. Women undergoing infertility treatments often experience high levels of stress, anxiety, and depression, stemming from the physical, emotional, and financial strains of the process. (23) The uncertainty and repeated cycles of hope and disappointment can exacerbate these feelings, leading to long-term psychological distress if not adequately addressed.
Mental health during pregnancy and the postpartum period is another critical area of concern. Pregnancy, while often a joyous time, can also be accompanied by anxiety and depression, which can persist or even intensify after childbirth. Postpartum depression (PPD) is a severe condition that affects many new mothers, characterized by sadness, fatigue, and difficulty bonding with the baby. (24) The risk factors for PPD include a history of depression, lack of support, and stressful life events during pregnancy. Addressing these mental health issues promptly is essential for the well-being of both the mother and the infant.
The emotional toll of pregnancy loss and stillbirth is profound, often leading to significant psychological distress, including depression, anxiety, and post-traumatic stress disorder (PTSD). The loss of a pregnancy or stillbirth is a traumatic event that can deeply affect a woman’s mental health, necessitating comprehensive support and counseling to navigate the grief and trauma associated with such loss. (25)
Efforts to improve mental health outcomes in these areas have included increased screening for psychological distress during and after pregnancy, better support systems for women undergoing ART, and more robust mental health services for those who have experienced pregnancy loss. Legislative efforts like the Black Maternal Health Momnibus Act aim to address these disparities and ensure that all women receive the mental health care they need during these critical times.
IV. Gynecologic Oncology and Mental Health
Women diagnosed with gynecologic cancers, such as ovarian, cervical, and endometrial cancers, face numerous psychological challenges. The diagnosis itself often brings intense fear and anxiety about the future, treatment outcomes, and potential loss of fertility, significantly impacting mental health. (26) These psychological burdens are compounded by the physical side effects of cancer and its treatments, including surgery, chemotherapy, and radiation, which can lead to body image issues, fatigue, and chronic pain, further exacerbating mental distress. (27)
Mental health support is crucial for women undergoing cancer treatment and survivorship. Effective mental health interventions include psychological counseling, support groups, and integrative therapies such as mindfulness and cognitive-behavioral therapy (CBT), which have been shown to alleviate anxiety, depression, and post-traumatic stress disorder (PTSD) related to cancer. (28) Survivorship care plans that include mental health resources are essential for helping women navigate the long-term psychological effects of cancer and its treatment. These plans can provide continuity of care and support the emotional and psychological needs of survivors as they transition from active treatment to post-treatment life. (29)
V. Sexual Health and Psychological Well-being
Sexual health is intricately linked to psychological well-being, and disruptions in sexual function can significantly impact mental health. Sexual dysfunction, including conditions such as vaginismus and dyspareunia, often leads to emotional distress, reduced self-esteem, and strained interpersonal relationships.
Sexual dysfunction can manifest in various forms, including difficulties with sexual desire, arousal, orgasm, and pain during intercourse. These issues are not merely physical but are deeply interwoven with psychological factors. Anxiety, depression, and stress are both causes and consequences of sexual dysfunction, creating a challenging cycle for affected individuals. For example, women experiencing chronic pain during intercourse, such as in dyspareunia, may develop anticipatory anxiety, leading to avoidance of sexual activity and further psychological distress. (22)
Addressing the psychological aspects of conditions like vaginismus and dyspareunia involves a multifaceted approach. Vaginismus, characterized by involuntary contractions of the vaginal muscles, often stems from anxiety or trauma. Psychological interventions, including cognitive-behavioral therapy (CBT) and sex therapy, are essential components of treatment. These therapies aim to reduce anxiety, reframe negative thought patterns, and gradually desensitize the individual to penetration. (22)
Dyspareunia, or painful intercourse, can have both physical and psychological origins. It is crucial to identify any underlying medical conditions, such as endometriosis or pelvic inflammatory disease, that might contribute to pain. Concurrently, addressing the psychological impact through counseling and therapy is vital. Women with dyspareunia often benefit from a supportive environment where they can discuss their experiences and receive validation and strategies to manage pain and anxiety.
VI. Mental Health Screening and Intervention in Gynecological Practice
Current practices and guidelines for mental health screening in gynecology emphasize the need for integrating mental health evaluations into routine gynecological care. The American College of Obstetricians and Gynecologists (ACOG) recommends that gynecologists should be proficient in recognizing and addressing mental health conditions, given the high prevalence of issues such as depression and anxiety among women. (30) Comprehensive mental health screening tools, like the Edinburgh Postnatal Depression Scale and the Patient Health Questionnaire-9 (PHQ-9), are suggested for use in clinical settings to identify women at risk of mental health disorders. (5)
Gynecologists often encounter patients dealing with significant life transitions or medical conditions that can exacerbate mental health issues, including pregnancy, menopause, and chronic gynecological conditions like endometriosis or polycystic ovary syndrome (PCOS). Integrative approaches that combine mental health services with gynecological care have shown promise in improving outcomes for these patients. For instance, collaborative care models where mental health professionals work alongside gynecologists can provide comprehensive care, addressing both physical and psychological needs. (31)
The implementation of these integrated care models requires overcoming barriers such as time constraints during patient visits, the stigma associated with mental health issues, and a lack of mental health training among gynecologists. Despite these challenges, studies suggest that such integrative approaches are essential for holistic patient care and can significantly improve quality of life for women suffering from both gynecological and mental health conditions. (32)
VII. The role of health care providers
The role of healthcare providers in addressing the intersection of gynecology and mental health is critical, and it begins with comprehensive training and education for gynecologists. The integration of mental health training into gynecology curricula has gained increasing attention, highlighting the necessity for gynecologists to be well-versed in identifying and managing mental health issues. Recent guidelines emphasize the importance of this interdisciplinary approach, ensuring that gynecologists are equipped with the skills to recognize mental health symptoms and provide appropriate referrals when necessary. (11)
Professional organizations and educational institutions are actively working to incorporate mental health training into gynecology programs. For instance, initiatives by the American College of Obstetricians and Gynecologists (ACOG) now include mental health modules as part of their continuing medical education (CME) requirements. These programs are designed to enhance gynecologists' understanding of the psychological impacts of gynecological conditions, such as anxiety and depression associated with chronic pelvic pain, infertility, and gynecologic cancers. (33)
Collaboration between gynecologists, psychiatrists, and psychologists is another essential aspect of providing holistic care to patients. This collaborative model is increasingly recognized as best practice, with studies demonstrating improved patient outcomes when mental health professionals are integrated into gynecological care teams. Such collaboration facilitates a more comprehensive approach to patient care, addressing both physical and psychological needs simultaneously. (34)
To support these efforts, several health systems have developed integrated care models where mental health services are embedded within gynecology clinics. This integration allows for seamless referrals and immediate mental health support, which is particularly beneficial for patients dealing with conditions that have significant psychological impacts, such as infertility treatments and cancer diagnoses. (35)
Furthermore, policy initiatives at the national and international levels are pushing for the adoption of mental health screening and intervention as a standard practice in gynecology. These initiatives stress the importance of mental health as a component of overall health and advocate for the necessary resources to support integrated care models.
VIII. Cultural and socioeconomic factors
Cultural and socioeconomic factors play significant roles in shaping women's access to gynecological and mental health care, influencing both their experiences and outcomes. Cultural attitudes towards gynecology and mental health can vary widely, affecting women's willingness to seek and adhere to treatment. In some cultures, stigma around mental health issues or gynecological conditions can discourage women from seeking care. For instance, traditional beliefs and societal norms may prioritize physical health over mental health, or view mental health issues as a source of shame. (13) This cultural stigma can lead to delayed diagnosis and treatment, worsening health outcomes.
Furthermore, cultural competence among healthcare providers is essential in addressing these barriers. Providers must be trained to understand and respect cultural differences, which can help in building trust and improving patient-provider communication. Initiatives to increase cultural competence in healthcare settings are vital for improving access and quality of care for diverse populations. (26)
Socioeconomic barriers also significantly impact access to integrated gynecological and mental health care. Economic constraints can limit access to healthcare services, including necessary screenings and treatments. Women from lower socioeconomic backgrounds may lack insurance coverage, face high out-of-pocket costs, or have limited access to healthcare facilities. These barriers are compounded by social determinants of health such as education, employment, and living conditions, which further exacerbate health disparities. (36)
Efforts to mitigate these barriers include policy interventions aimed at improving healthcare affordability and accessibility, such as expanding insurance coverage and providing financial assistance programs. Additionally, community-based programs that offer integrated care services in accessible locations can help address both economic and cultural barriers. Collaborative approaches that involve community stakeholders in the planning and implementation of healthcare services are crucial for ensuring that these services are both effective and culturally appropriate. (11, 36)
IX. Future Directions
Emerging research and innovative approaches in gynecology and mental health highlight the increasing integration of advanced technologies and novel methodologies to enhance women's health outcomes. The rapid advancements in digital health, particularly the use of artificial intelligence (AI), telemedicine, and mobile health applications, have transformed the landscape of gynecological care. These technologies are being employed to improve the diagnosis, treatment, and monitoring of various gynecological conditions while addressing the psychological aspects associated with these health issues. For instance, AI-driven tools are being developed to provide personalized mental health support and to predict mental health conditions based on patient data. (35)
Innovative approaches such as the use of digital therapeutics and virtual reality (VR) are also gaining traction in the field. Digital therapeutics, which involve software-based interventions to prevent, manage, or treat medical conditions, are being utilized to address mental health issues like anxiety and depression among women with gynecological conditions. VR, on the other hand, is being explored as a tool for pain management and for reducing anxiety during gynecological procedures. (37)
Furthermore, there is a growing emphasis on the development of integrative care models that combine traditional gynecological practices with mental health services. These models aim to provide holistic care by incorporating mental health screening and interventions into routine gynecological visits. This approach not only helps in the early detection of mental health issues but also ensures timely and appropriate treatment, thereby improving overall health outcomes for women. (38)
The integration of mental health into gynecological care is also supported by policy changes and recommendations from global health organizations. These policies advocate for the inclusion of mental health training in the education of gynecologists and the establishment of collaborative care networks involving gynecologists, psychiatrists, and psychologists. Such collaborative efforts are crucial in providing comprehensive care that addresses both physical and mental health needs.
CONCLUSION
In conclusion, this literature review highlights the intricate relationship between gynecology and mental health, emphasizing the need for comprehensive care that addresses both physical and psychological dimensions of women's health. Key findings indicate that hormonal fluctuations, gynecological conditions, reproductive health issues, and gynecologic oncology significantly impact mental well-being. Cultural and socioeconomic factors further influence access to integrated care, underscoring the importance of culturally competent and accessible healthcare services. The integration of mental health screening and collaborative care models in gynecological practice is essential for improving patient outcomes. As emerging research and innovative approaches continue to evolve, the adoption of holistic care models that include mental health considerations remains crucial for advancing women's health and well-being.
BIBLIOGRPHICS REFERENCES
1. Brown L, Hunter MS, Chen R, Crandall CJ, Gordon JL, Mishra GD, et al. Promoting good mental health over the menopause transition. Lancet [Internet]. 2024 [cited 31/03/2024]; 403(10430):969-983. Available in: https://doi.org/10.1016/S0140-6736(23)02801-5
2. Carlini SV, Deligiannidis KM. Evidence-Based Treatment of Premenstrual Dysphoric Disorder: A Concise Review. J Clin Psychiatry [Internet]. 2020 [cited 21/03/2024]; 81(2):19ac13071. Available in: https://doi.org/10.4088/JCP.19ac13071
3. Till SR, As-Sanie S, Schrepf A. Psychology of Chronic Pelvic Pain: Prevalence, Neurobiological Vulnerabilities, and Treatment. Clin Obstet Gynecol [Internet]. 2019 [cited 29/03/2024]; 62(1):22-36. Available in: https://doi.org/10.1097/GRF.0000000000000412
4. La Rosa VL, De Franciscis P, Barra F, Schiattarella A, Török P, Shah M, et al. Quality of life in women with endometriosis: a narrative overview. Minerva Medica [Internet]. 2020 [cited 25/03/2024]; 111(1):68–78. Available in: https://doi.org/10.23736/S0026-4806.19.06298-0
5. Yang K, Wu J, Chen X. Risk factors of perinatal depression in women: a systematic review and meta-analysis. BMC Psychiatry [Internet]. 2022 [cited 05/03/2024]; 22(1):63. Available in: https://doi.org/10.1186/s12888-021-03684-3
6. Patel A, Sharma PSVN, Kumar P. "In Cycles of Dreams, Despair, and Desperation:" Research Perspectives on Infertility Specific Distress in Patients Undergoing Fertility Treatments. Journal of Human Reproductive Sciences [Internet]. 2018 [cited 13/04/2024]; 11(4):320–328. Available in: https://doi.org/10.4103/jhrs.JHRS_42_18
7. Nasution LA, Afiyanti Y, Ma’rifah AR. The most unmet needs on Gynecological and Breast Cancer Survivors, A Systematic Review. Enfermería Global [Internet]. 2023 [cited 04/03/2024]; 22(2):497–521. Available in: https://doi.org/10.6018/eglobal.530511
8. Ma'rifah AR, Afiyanti Y, Huda MH, Chipojola R, Putri YR, Nasution MAT. Effectiveness of psychoeducation intervention among women with gynecological cancer: a systematic review and meta-analysis of randomized controlled trials. Supportive Care in Cancer [Internet]. 2022 [cited 19/03/2024]; 30(10):8271–8285. Available in: https://doi.org/10.1007/s00520-022-07277-y
9. Adebisi OY, Carlson K. Hypoactive Sexual Desire Disorder in Women. StatPearls Publishing [Internet]. 2024 [cited 24/03/2024]. Available in: https://www.ncbi.nlm.nih.gov/books/NBK603746/
10. Miller ES, Jensen R, Hoffman MC, Osborne LM, McEvoy K, Grote N, et al. Implementation of perinatal collaborative care: a health services approach to perinatal depression care. Primary Health Care Research & Development [Internet]. 2020 [cited 17/03/2024]; 21. Available in: https://doi.org/10.1017/S1463423620000110
11. Brindis CD, Laitner MH, Clayton EW, Scrimshaw SC, Grosz BJ, Simpson LA, et al. Health-care workforce implications of the Dobbs v Jackson Women's Health Organization decision. Lancet [Internet]. 2024 [cited 30/03/2024]; 403(10445):2747–2750. Available in: https://doi.org/10.1016/S0140-6736(24)00581-6
12. Geraghty L. Homelessness facts and statistics: The numbers you need to know in 2024. Big Issue [Internet]. 2024 [cited 03/02/2024]. Available in: https://www.bigissue.com/news/housing/britains-homelessness-shame-cold-hard-facts/#:~:text=A%20total%20of%204%2C118%20people,statistics%20have%20taken%20its%20place
13. Raney JH, Weinstein S, Ganson KT, Testa A, Jackson DB, Pantell M, et al. Mental Well-Being Among Adversity-Exposed Adolescents During the COVID-19 Pandemic. JAMA Network Open [Internet]. 2024 [cited 13/04/2024]; 7(3). Available in: https://doi.org/10.1001/jamanetworkopen.2024.2076
14. Raney JH, Weinstein S, Ganson KT, Testa A, Jackson DB, Pantell M, et al. In the Face of Adversity: Pandemic Mental Health Protective Factors for Adolescents Who Have Experienced Adverse Childhood Experiences. Journal of Adolescent Health [Internet]. 2024 [cited 11/04/2024]; 74(3). Available in: https://doi.org/10.1016/j.jadohealth.2023.11.305
15. Ma S, Song SJ. Oral contraceptives containing drospirenone for premenstrual syndrome. Cochrane Database Syst Rev [Internet]. 2023 [cited 26/02/2024]; 6(6):CD006586. Available in: https://doi.org/10.1002/14651858.CD006586.pub5
16. Zethraeus N, Kocoska-Maras L, Ellingsen T, von Schoultz B, Hirschberg AL, Johannesson MA. A randomized trial of the effect of estrogen and testosterone on economic behavior. Proceedings of the National Academy of Sciences of the United States of America [Internet]. 2009 [cited 23/04/2024]; 106(16):6535–6538. Available in: https://doi.org/10.1073/pnas.0812757106
17. Mu E, Kulkarni J. Hormonal contraception and mood disorders. Australian Prescriber [Internet]. 2022 [cited 01/03/2024]; 45(3):75-79. Available in: https://doi.org/10.18773/austprescr.2022.025
18. Maki PM, Kornstein SG, Joffe H, Bromberger JT, Freeman EW, Athappilly G, et al. Guidelines for the Evaluation and Treatment of Perimenopausal Depression: Summary and Recommendations. Journal of Women's Health [Internet]. 2019 [cited 22/02/2024]; 28(2):117-134. Available in: https://doi.org/10.1089/jwh.2018.27099.mensocrec
19. Namazi M, Behboodi Moghadam Z, Zareiyan A, Jafarabadi M. Exploring the impact of endometriosis on women's lives: A qualitative study in Iran. Nurs Open [Internet]. 2021 [cited 15/03/2024]; 8(3):1275-1282. Available in: https://doi.org/10.1002/nop2.744
20. Yin X, Ji Y, Chan CLW, Chan CHY. The mental health of women with polycystic ovary syndrome: a systematic review and meta-analysis. Arch Womens Ment Health [Internet]. 2021 [cited 02/02/2024]; 24(1):11-27. Available in: https://doi.org/10.1007/s00737-020-01043-x
21. Chiuve SE, Huisingh C, Petruski-Ivleva N, Owens C, Kuohung W, Wise LA. Uterine fibroids and incidence of depression, anxiety and self-directed violence: a cohort study. Journal of Epidemiology and Community Health [Internet]. 2022 [cited 04/03/2024]; 76(1):92–99. Available in: https://doi.org/10.1136/jech-2020-214565
22. South & West. 7.4.2 Drugs for urinary frequency, enuresis, and incontinence. South & West [Internet].2024 [cited 30/03/2024]. Available in: https://southwest.devonformularyguidance.nhs.uk/formulary/chapters/7-obstetrics-gynaecology-and-urinary-tract-disorders/7-4-genito-urinary-disorders/7-4-2-drugs-for-urinary-frequency-enuresis-and-incontinence
23. Rooney KL, Domar AD. The relationship between stress and infertility. Dialogues in Clinical Neuroscience [Internet]. 2018 [cited 22/02/2024]; 20(1):41–47. Available in: https://doi.org/10.31887/DCNS.2018.20.1/klrooney
24. Lewkowitz AK, Whelan AR, Ayala NK, Hardi A, Stoll C, Battle CL, et al. The effect of digital health interventions on postpartum depression or anxiety: a systematic review and meta-analysis of randomized controlled trials. American Journal of Obstetrics and Gynecology [Internet]. 2024 [cited 23/03/2024];230(1):12–43. Available in: https://doi.org/10.1016/j.ajog.2023.06.028
25. Mughal S, Azhar Y, Siddiqui W. Postpartum Depression. StatPearls [Internet]. 2022 [cited 26/02/2024]. Available in: https://www.ncbi.nlm.nih.gov/books/NBK519070/
26. Global Cancer Observatory [Internet]. 2024 [cited 04/03/2024]. Available in: https://gco.iarc.fr/en
27. Zhao J, Kong Y, Xiang Y, Yang J. The research landscape of the quality of life or psychological impact on gynecological cancer patients: A bibliometric analysis. Frontiers in Oncology [Internet]. 2023 [cited 16/02/2024]; 13. Available from: https://doi.org/10.3389/fonc.2023.1115852
28. Hack C, Hüttner N, Paepke D, Voiß P, Dobos G, Kümmel S, et al. Integrative Medizin in der Gynäkologischen Onkologie – Möglichkeiten und Grenzen Teil 1. Tumordiagnostik & Therapie [Internet]. 2014 [cited 28/03/2024]; 35(06):337–344. Available in: https://doi.org/10.1055/s-0034-1385131
29. de Rooij BH, Thomas TH, Post KE, Flanagan J, Ezendam NPM, Peppercorn J, et al. Survivorship care planning in gynecologic oncology-perspectives from patients, caregivers, and health care providers. Journal of Cancer Survivorship [Internet]. 2018 [cited 06/02/2024]; 12(6):762–774. Available in: https://doi.org/10.1007/s11764-018-0713-9
30. ACOG Committee Opinion No. 757: Screening for Perinatal Depression. Obstet Gynecol [Internet]. 2018 [cited 30/03/2024]; 132(5)–e212. Available in: https://doi.org/10.1097/AOG.0000000000002927
31. World Health Organization. Integrating the social determinants of health into health workforce education and training [Internet]. 2023 [cited 06/02/2024]. Available in: https://www.who.int/news-room/events/detail/2023/11/08/default-calendar/integrating-the-social-determinants-of-health-into-health-workforce-education-and-training
32. Chen W, Peng W, Zhang Y, Zhou H, Zhang M. Anxiety and depression among perinatal women during the long-term normal prevention of COVID-19 pandemic period in China: a cross-sectional study. BMC Psychiatry [Internet]. 2023 [cited 29/02/2024]; 23(1):451. Available in: https://doi.org/10.1186/s12888-023-04930-6
33. American Medical Association. Integrating mental health care into the OB practice [Internet]. 2022 [cited 05/03/2024]. Available in: https://www.ama-assn.org/about/events/integrating-mental-health-care-ob-practice
34. Selix N, Henshaw E, Barrera A, Botcheva L, Huie E, Kaufman G. Interdisciplinary Collaboration in Maternal Mental Health. MCN the American Journal of Maternal/Child Nursing [Internet]. 2017 [cited 12/03/2024]; 42(4):226–231. Available in: https://doi.org/10.1097/nmc.0000000000000343
35. World Health Organization. WHO unveils a digital health promoter harnessing generative AI for public health [Internet]. 2024 [cited 28/02/2024]. Available in: https://www.who.int/news/item/02-04-2024-who-unveils-a-digital-health-promoter-harnessing-generative-ai-for-public-health
36. GOV.UK. Keeping children safe in education [Internet]. 2024 [cited 05/03/2024]. Available in: https://www.gov.uk/government/publications/keeping-children-safe-in-education--2
37. World Health Organization. World health statistics 2024: monitoring health for the SDGs, sustainable development goals [Internet]. 2024 [cited 29/02/2024]. Available in: https://www.who.int/publications/i/item/9789240094703
38. U.S. Agency for International Development. Digital Strategy 2020-2024 [Internet]. 2024 [cited 01/03/2024]. Available in: https://www.usaid.gov/digital-development/digital-strategy#:~:text=USAID's%20first%20Digital%20Strategy%20charts,development%20and%20humanitarian%20assistance%20outcomes
AUTHORSHIP CONTRIBUTION
KE: Conceptualization, data curation, formal analysis, investigation, methodology, resources, supervision, validation, visualization, original draft writing, writing and editing.
CONFLICT OF INTERESTS
The author declare that they have no conflicts of interest.
SOURCES OF FUNDING
The author did not receive funding for the development of this article.