ORIGINAL ARTICLE
Epidemiological behavior of pregnant women with syphilis in the Julián Grimau health area during the 2021-2022 period
Comportamiento epidemiológico de las gestantes con sífilis en el período de 2021-2022 del área de salud Julián Grimau
María Dolores Malfrán García 1*, https://orcid.org/0000-0003-2124-5579
Laineris Núñez Odilio 1, https://orcid.org/0000-0003-2124-5579
Dayma León Bueno 1, https://orcid.org/0000-0003-2124-5579
Ekaterine Zayas Tamayo 1, https://orcid.org/0000-0003-2797-2849
Carlos David Boris Miclín 1, https://orcid.org/0009-0003-7658-7645
1 University of Medical Sciences of Santiago de Cuba. Faculty of Medicine No. 2, Santiago de Cuba, Cuba
* Corresponding author: doloresmalfran@infomed.sld.cu
Received: 20/09/2024
Accepted: 17/02/2025
How to cite this article: Malfrán-García MD, Núñez-Odilio L, León-Bueno D, Zayas-Tamayo E, Boris-Miclín CD. Epidemiological behavior of pregnant women with syphilis in the Julián Grimau health area during the 2021-2022 period. MedEst. [Internet]. 2025 [cited access date]; 5:e323. Available in: https://revmedest.sld.cu/index.php/medest/article/view/323
ABSTRACT
Introduction: syphilis is a curable infection caused by Treponema pallidum, it is transmitted sexually and also, during pregnancy, from the mother to the fetus.
Objective: to describe the epidemiological profile of pregnant women with syphilis in the period 2021-2022 of the Julián Grimau health area, of the Santiago de Cuba municipality.
Methods: an observational, descriptive and cross-sectional study was carried out in the Julián Grimau health area, in the Santiago de Cuba municipality in the period 2021-2022. The population consisted of 26 pregnant women reported with syphilis in the study period. Quantitative and qualitative variables were used, taking into account their operational definition, scale and form of measurement.
Results: the most represented ages were 15-19 years, 79,6 % of pregnant women had uptake with less than 14 weeks of gestation, 69,2 % of pregnant women had reactive VDRL results of 16-32 dill; 19,2 % took more than 7 days between the reactive result and the treatment applied, 76,9 % showed positive TPHA results in pregnant women, 61,5 % of pregnant women confirmed with Early Acquired Latent Syphilis (STAL) predominate.
Conclusions: the lack of detection or study of couples, as well as the delay and lack of opportunity in indicating and giving treatment to them and to pregnant women with reactive serologies, can ruin the prevention of syphilis and vertical transmission of this infection.
Keywords: Pregnant Women; Syphilis; Couples; Treatment
RESUMEN
Introducción: la sífilis es una infección curable causada por el Treponema pallidum, se trasmite por vía sexual y también, durante el embarazo, de la madre al feto.
Objetivo: describir el perfil epidemiológico de las gestantes con sífilis en el período de 2021-2022 del área de salud Julián Grimau, del municipio Santiago de Cuba.
Métodos: se realizó un estudio observacional, descriptivo y de corte transversal en área de salud Julián Grimau, del municipio Santiago de Cuba en el período de 2021-2022. La población estuvo constituida por 26 gestantes notificadas con sífilis en el período de estudio. Se utilizaron variables cuantitativas y cualitativas, teniendo en cuenta su definición operacional, la escala y forma de medición.
Resultados: las edades más representada fueron de 15–19 años, el 79,6 % de las gestantes tuvieron captación con menos de 14 semanas de gestación, el 69,2 % de las gestantes tuvieron resultados de VDRL reactiva de 16–32 dill; el 19,2 % demoró más de 7 días entre el resultado reactivo y el tratamiento aplicado, el 76,9 % arrojó resultados positivos de TPHA en gestantes, predominan el 61,5 % de las gestantes confirmadas con Sífilis Temprana Adquirida Latente (STAL).
Conclusiones: la no detección, ni estudio de las parejas, así como la demora y falta de oportunidad en indicar y poner el tratamiento a éstos y a las embarazadas con serologías reactivas, pueden dar al traste con la prevención de la sífilis y con la transmisión vertical de esta infección.
Palabras clave: Gestantes; Sífilis; Parejas; Tratamiento
INTRODUCTION
Sexually transmitted infections (STIs) constitute a significant public health problem worldwide, affecting quality of life and accompanied by high levels of morbidity and mortality. These infections directly impact child and reproductive health as they lead to infertility, cancers, and pregnancy complications. (1)
Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum, subspecies pallidum. Transmission occurs primarily through sexual contact (oral, vaginal, or anal). It can also be transmitted vertically, with a fetal mortality rate exceeding 40 %. Most people with syphilis are asymptomatic, which contributes to maintaining the chain of transmission. If left untreated, the disease can progress to severe systemic complications several years after the initial infection. (2)
Untreated gestational syphilis can lead to serious complications such as spontaneous abortion, stillbirth, neonatal death, preterm birth, low birth weight, and congenital infection with varying degrees of severity. Despite the existence of effective prevention measures and relatively inexpensive treatment options, syphilis remains a global public health problem. (3)
According to the World Health Organization, an estimated 7 million people contract syphilis each year, and mother-to-child transmission of syphilis continues to be a significant cause of perinatal morbidity and mortality. In 2020, mother-to-child transmission of syphilis caused approximately 200,000 fetal and neonatal deaths, as well as 350,000 cases of congenital syphilis worldwide. (4)
In Latin America and the Caribbean, congenital syphilis remains a significant problem. According to data from the Pan American Health Organization (PAHO, 2021), an estimated 200 000 to 400 000 children are born with congenital syphilis each year in the region. In Brazil, for example, in 2020, 158 000 cases of acquired syphilis, 62 000 cases of syphilis in pregnant women, and 24 000 cases of congenital syphilis were reported, according to the Notifiable Diseases Information System (SINAN). Additionally, between 1998 and 2020, 2 800 deaths due to congenital syphilis were recorded in children under one year of age. (5)
In the United States, congenital syphilis has seen an alarming increase in recent years. According to the Centers for Disease Control and Prevention (CDC, 2021), between 2016 and 2020, cases of congenital syphilis increased by 235 %, with a rate of 59,4 cases per 100 000 live births in 2020. This increase has been attributed to the lack of access to screening and timely treatment during pregnancy. (6)
In Cuba, maternal and child health care remains a national priority. According to the Cuban Ministry of Public Health, the country has maintained significant achievements in reducing infant mortality and eliminating vertical transmission of HIV and congenital syphilis. In 2020, Cuba's infant mortality rate was 4,9 per 1,000 live births, and zero cases of vertical transmission of congenital syphilis were reported, confirming the sustainability of the achievements since the certification of elimination in 2015. (7)
Cuba was the first country in the world to receive validation for the elimination of mother-to-child transmission of HIV and congenital syphilis from the Pan American Health Organization (PAHO) and the World Health Organization (WHO) in 2015. This achievement was the result of a coordinated national effort, including the implementation of the National Maternal and Child Health Program and ensuring equitable access to health services. During the validation process, three provinces were selected, including Santiago de Cuba, where the José Martí and 28 de Septiembre health areas were audited and met the established criteria for certification. (7)
The province of Santiago de Cuba was one of those selected to represent the country in this process, with a syphilis prevalence in pregnant women of 0.23 and 0.24 in 2012, 0.17 and 0.18 in 2013, and 0.18 and 0.19 % in 2014, respectively. The rates and cases of congenital syphilis were 0.0 in 2012 (0 cases), 0.07 in 2013 (1 case), and 0.07 per 1,000 live births in 2014 (1 case). Regarding HIV transmission, the prevalence of HIV in pregnant women detected positive for HIV in prenatal screening/live births during the period was 0.03 %, 0.05 %, and 0.04 % in 2012, 2013, and 2014, respectively. The prevalence of HIV in pregnant women among all those who were pregnant during the period/live births was 0.16 %, 0.18 %, and 0.14 % in the same period. The rates and cases of mother-to-child transmission (MTCT) of HIV were 0 cases % in all three years (2012-2014), with some indicators slightly higher than the national average but still well below the thresholds required for certification. (Data from the presentation: Experiences of Santiago de Cuba Province in the Validation of the Strategy for the Elimination of MTCT of HIV and Congenital Syphilis). (7)
Impact and coverage indicators have remained fulfilled in the following years up to the present. By the end of 2020, the province diagnosed 521 cases of syphilis, of which 44 were in pregnant women, out of a total of 12 447 pregnant women screened, resulting in a prevalence rate of 0.35 per 100. There were no cases of congenital syphilis. (Data collected from the 2020 Provincial Report of the STI Program of the CPHEM of Santiago de Cuba). (7)
In the Julián Grimau Health Area, according to data from the STI Report of the health area, in 2020, 17 cases of syphilis were reported in the population, of which 4 were pregnant women, out of a total of 12 pregnant women with reactive syphilis serology out of 497 screened during the year, resulting in a prevalence rate of 0.8 per 100. There were no cases of congenital syphilis, but this risk of syphilis in pregnant women was higher than the provincial average and higher than the area's results in 2019.
Given the above, a research study is being conducted with the aim of describing the epidemiological profile of pregnant women with syphilis in the Julián Grimau Health Area during the period 2021-2022.
METHODOLOGICAL DESIGN
An observational, descriptive, cross-sectional study was conducted in the Julián Grimau Health Area of the Santiago de Cuba municipality during the 2021-2022 period.
The population and sample consisted of 26 pregnant women, representing all pregnant women notified with syphilis during the study period who were treated, resided, and were registered in the time series of the STI and Statistics Departments of the Julián Grimau Polyclinic. No sample was used.
The variables analyzed were: age, distributed in 5-year intervals (15-19 years, 15-19 years, 15-19 years, 15-19 years, 15-19 years, 15-19 years, 15-19 years).
This research took into account the bioethical principles and guidelines established when human subjects participated in the study, namely: the Nuremberg Code since 1947; the Helsinki Declaration in Finland, promulgated since 1964, and approved in Tokyo, Japan, in October 1975; the 35th International Conference on Human Rights in Venice, Italy, in October 1983; the 41st in Hong Kong in September 1989, and the 52nd General Assembly in Edinburgh, Scotland, in October 2000.
The guidelines of other relevant documents were also followed, such as the International Guidelines for Biomedical Research Involving Human Subjects, proposed in 1982 by the Council for International Organizations of Medical Sciences (COICM) and the World Health Organization (WHO).
A meeting was held with the directors of the "Julián Grimau" health department, where they were informed about the research and its objectives, their approval was requested, and its importance was demonstrated.
RESULTS
Table 1 shows the age groups in years completed among pregnant women with syphilis in the Julián Grimau health area. The predominant age groups were 15–19 and 25–29, representing 30.8%. The age distribution in this study corresponded to the ages of peak sexual activity and the average age at which pregnancies are achieved in our country.
Table 1: Age distribution of pregnant women with syphilis at the Julián Grimau Polyclinic in the municipality of Santiago de Cuba, 2021–2022.
|
Age Group |
No |
% |
|
15- 19 |
8 |
30,8 |
|
20 - 24 |
7 |
26,9 |
|
25 - 29 |
8 |
30,8 |
|
30 - 34 |
2 |
7,7 |
|
35 - 39 |
1 |
3,8 |
|
40 - 44 |
0 |
0,0 |
|
45 y más |
0 |
0,0 |
|
Total |
26 |
100,0 |
Source: Register of Pregnant Women Captured, Department of STIs
Chart 1 shows that 76.9% (20) of the pregnant women were recruited in the first trimester, with a gestational age of 13.6 weeks or less.
Chart 1: Distribution by gestational age at pregnancy recruitment
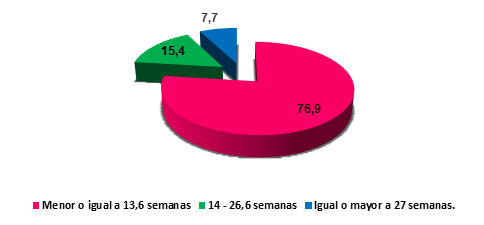
Source: Register of Pregnant Women Captured, Department of STIs
Table 2 shows that 69.2% of pregnant women had reactive VDRL results of 16–32 dilutions (dilutions).
Table 2: Distribution by VDRL Results
|
VDRL Results |
Pregnant women |
|
|
No |
% |
|
|
Weak Reactive |
2 |
7,7 |
|
Less than 8 dil |
6 |
23,1 |
|
16 - 32 dil |
18 |
69,2 |
|
Greater than 32 dil |
0 |
0,0 |
|
Total |
26 |
100,0 |
Source: Register of Pregnant Women Captured, Department of STIs
Table 3 shows the time between the date of the reactive result and the date of treatment. As can be seen, 53.8% were treated within 1-3 days, or within the first 72 hours. 19.2% took 7 days or more, even though the National Endocrinology Program (PEN) establishes that pregnant women with reactive serology are monitored by the first physician who receives the result.
Table 3: Distribution according to the time between the reactive result and the treatment applied.
|
Time |
Pregnant women |
|
|
No |
% |
|
|
1-3 days |
14 |
53,8 |
|
4-6 days |
7 |
26,9 |
|
7 days or more |
5 |
19,2 |
|
Total |
26 |
100,0 |
Source: Register of Pregnant Women Captured, Department of STIs
Table 4 shows that 76.9% of pregnant women had positive TPHA (Treponema Pallidum Hem Agglutination Test) results, and 19.2% had not received a test at the time of the study.
Table 4: Distribution by TPHA Results
|
TPHA Results |
Pregnant women |
|
|
No |
% |
|
|
Positive |
20 |
76,9 |
|
Negative |
0 |
0,0 |
|
Not Performed |
5 |
19,2 |
|
Results Pending |
1 |
3,8 |
|
Total |
26 |
100,0 |
Source: Register of Pregnant Women Captured, Department of STIs
Chart 2 shows that pregnant women confirmed with Latent Early Acquired Syphilis (STAL) predominate (61.5%). Of the 38.5% of cases of Symptomatic Early Acquired Syphilis (STAL), 60% (6) are due to cutaneous symptoms.
Chart 2: Distribution according to pregnant women confirmed by diagnostic conclusion
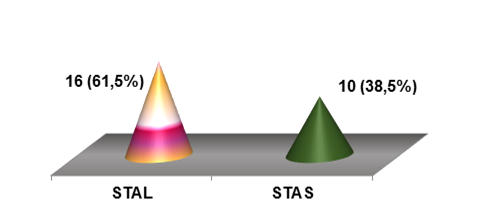
Source: Register of Pregnant Women Captured, Department of STIs
DISCUSSION
In the study by Gutiérrez Brenes et al. (8), titled “Congenital Syphilis: A Deceptive Disease”, it was found that most cases of gestational syphilis were diagnosed in women between 18 and 34 years of age, coinciding with the onset of sexual activity and a higher birth rate. These findings are consistent with the results of the present study, where the most affected age groups were 15-19 and 25-29 years, suggesting that women of active reproductive age are the most vulnerable to this infection.
For their part, Silva Giordana et al. (9), in their research “Syphilis in Pregnant Women and Congenital Syphilis: Epidemiological Profile and Prevalence”, reported that more than half of pregnant women with syphilis were in the 20 to 34 age range and predominantly belonged to the white race. Additionally, they highlighted that these women had more than three years of education, indicating that while education can be a protective factor, it is not sufficient to prevent infection in all cases. These results partially contrast with the present study, where the educational level of pregnant women was not analyzed, but a predominance of young women was observed, reinforcing the need to strengthen prevention strategies in this age group.
In the study by Benítez J et al. (10), “Sociodemographic and Clinical Characteristics of Gestational Syphilis in Cali, 2018”, it was found that out of 171 pregnant women, only 37 began prenatal care between the first and second trimesters (12-13 weeks). Furthermore, in 8 of these women, the treponemal test was performed late, between weeks 17 and 31, when the ideal is to conduct it at the start of prenatal care. Additionally, it was reported that 51.5% of pregnant women did not receive the full penicillin treatment, and only 57.6% of their sexual partners were treated. These findings highlight the importance of early detection and timely treatment, both for pregnant women and their partners, to prevent vertical transmission of syphilis.
Prenatal care should begin within the first 12 weeks of gestation, and the first syphilis screening test should be conducted as early as possible during pregnancy. It is crucial that, in the presence of any genital or generalized skin lesions, syphilis be ruled out through specialized clinical evaluation. In populations with a high prevalence of syphilis, it is recommended to repeat the screening test at the start of the third trimester (week 28) and at the time of delivery. (11)
In clinical practice, there are various diagnostic tests that, along with a comprehensive clinical evaluation, allow for an accurate diagnosis of syphilis. Currently, non-treponemal serological tests, such as VDRL and RPR (rapid plasma reagin), and treponemal tests, such as FTA-ABS and MHA-TP, are used. According to Guzmán M et al. (12), in their study “False Reactive VDRL Tests in Syphilis Management: False Positive Reactions in Pregnancy”, 4,344 serum samples from pregnant women were analyzed, of which 64 were VDRL reactive but FTA-ABS non-reactive, representing 1.5% of false positives. Additionally, 25 cases of confirmed syphilis (0.6%) were identified. False positive reactions were primarily associated with the first pregnancy and occurred at low titers (0-2 dilutions).
Benzathine penicillin is the only effective treatment for syphilis in pregnant women, as it crosses the placental barrier and treats both the mother and the fetus. Penicillin administration should be carried out in healthcare facilities, and it is essential to maintain a seven-day interval between doses to ensure treatment effectiveness. Although anaphylactic reactions to penicillin are rare (0.002% of cases), it is crucial to monitor patients and actively search for those who do not complete the treatment regimen. (13)
In this study, 100% of pregnant women with reactive serology received appropriate treatment: 92.3% with benzathine penicillin as the first option and 7.7% with ceftriaxone due to penicillin allergies, following the recommendations of the STI Strategic Plan. (14-15)
The effectiveness of penicillin in curing syphilis in pregnant women and preventing congenital syphilis was established in the 1940s, before the widespread use of randomized controlled trials. Although the incidence of syphilis is low in developed countries, it remains a significant problem in developing countries, especially in regions with a high prevalence of HIV/AIDS. (16)
Treatment with medications other than benzathine penicillin during pregnancy is considered inadequate for preventing mother-to-child transmission. Additionally, maternal treatment is only considered adequate if initiated within 30 days after delivery and if the full cycle is administered according to the clinical stage of syphilis. Pregnant women who do not meet these criteria are classified as inadequately treated, and their newborns must be evaluated as cases of congenital syphilis and reported epidemiologically. (16)
During the first prenatal visit, it is recommended to request non-treponemal tests for women without risk factors and treponemal tests for those with risk factors, such as low educational level, low socioeconomic status, residence in areas with high syphilis morbidity, or risky behaviors. Non-treponemal tests, such as VDRL and RPR, are used to monitor treatment effectiveness and detect infection, while treponemal tests confirm the diagnosis. However, non-treponemal tests may yield false positives due to autoimmune disorders, infections, or pregnancy. (17)
It is important to consider the prozone phenomenon in non-treponemal tests, which can generate false negative results in RPR. This phenomenon is associated with secondary syphilis and pregnancy. (18) Syphilis can present symptomatically (primary, secondary, or tertiary) or asymptomatically (latent). However, when a patient with syphilis becomes pregnant or acquires the infection during pregnancy, gestational syphilis develops. Mother-to-fetal transmission can occur in any trimester, being more frequent in the early stages of the disease (70-100% in primary syphilis and 40% in early latent syphilis). Even in cases of tertiary syphilis, cases of congenital syphilis have been reported. (19,20)
The risk of transmission to the fetus varies depending on the type of syphilis: it is 60% in primary or secondary syphilis, 40% in early latent syphilis, and 8% in late latent syphilis. Therefore, the evaluation and treatment of the sexual partners of pregnant women are crucial to interrupting the chain of transmission of the infection.
The findings of this study highlight the importance of early detection and timely treatment of syphilis in pregnant women, especially in young women of reproductive age. The lack of testing and treatment of partners, as well as delays in treatment administration, can undermine efforts to prevent vertical transmission of syphilis.
It is essential to strengthen prenatal care strategies, ensure access to reliable diagnostic tests, and guarantee compliance with benzathine penicillin treatment, the only effective medication for preventing congenital syphilis. The evaluation and treatment of sexual partners are also crucial to interrupting the chain of transmission and maintaining achievements in the elimination of congenital syphilis.
CONCLUSIONS
Timely diagnosis of syphilis in pregnant women through serological testing is essential to maintain the elimination of vertical transmission of congenital syphilis. In the Julián Grimau Health Area, pregnant women diagnosed with syphilis were predominantly young, with a medium educational level, and accompanied by their partners, and most were detected early during pregnancy. However, the lack of detection and evaluation of partners, as well as delays in prescribing and administering treatment to both pregnant women and their partners, can compromise prevention efforts and increase the risk of vertical transmission of the infection.
BIBLIOGRAPHIC REFERENCES
1. Ávila-Nieto C, Pedreño-López N, Mitjà O, Clotet B, Blanco J, Carrillo J. Syphilis vaccine: challenges, controversies and opportunities. Front Immunol. 2023 [cited 20/09/2024]; 14:1126170. Available in: https://pubmed.ncbi.nlm.nih.gov/37090699/
2. Pascoal LB, Carellos EVM, Tarabai BHM, et al. Maternal and perinatal risk factors associated with congenital syphilis. Trop Med Int Health. 2023 [cited 20/09/2024]; 28(6):442-453. Available in: https://pubmed.ncbi.nlm.nih.gov/37156513/
3. Mercuri SR, Moliterni E, Cerullo A, et al. Syphilis: a mini review of the history, epidemiology and focus on microbiota. New Microbiol. 2022 [cited 20/09/2024]; 45(1):28-34. Available in: https://pubmed.ncbi.nlm.nih.gov/35403844/
4. Organización Mundial de la Salud (OMS). (2022). Global progress report on HIV, viral hepatitis and sexually transmitted infections. Available in: https://www.who.int/publications/i/item/9789240053779
5. Organización Panamericana de la Salud (OPS). (2021). Epidemiological Update: Syphilis in the Americas. Available in: https://iris.paho.org/handle/10665.2/56085
6. Centers for Disease Control and Prevention (CDC). (2021). Sexually Transmitted Disease Surveillance 2020. Available in: https://www.cdc.gov/sti-statistics/media/pdfs/2024/07/2021-STD-Surveillance-Report-PDF_ARCHIVED-2-16-24.pdf
7. Anuario Estadístico de Salud 2021. MINSAP. Available in: https://files.sld.cu/dne/files/2022/10/Anuario-Estad%C3%ADstico-de-Salud-2021.-Ed-2022.pdf
8. Gutiérrez Brenes LJ, Víquez Quesada M, Valverde Chinchilla K. Sífilis congénita: una enfermedad engañosa . Rev.méd.sinerg. [Internet]. 2022 [cited 20/09/2024];7(6):e846. Available in: https://revistamedicasinergia.com/index.php/rms/article/view/846
9. Silva Giordana M, Pesce GB, Martins DC, Prado CM, Fernandes Carlos AM. Sífilis en la gestante y congénita: perfil epidemiológico y prevalencia. Enferm. glob. [Internet]. 2020 [cited 20/09/2024]; 19(57):107-150. Available in: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1695-61412020000100004&lng=es
10. Benítez J, Yépez MA, Hernández-Carrillo M, Martínez DM, Cubides-Munevar Á, Holguín-Ruiz JA, et al. Sociodemographic and clinical characteristics of gestational syphilis in Cali, 2018. Biomedica. 2021 [cited 20/09/2024]; 41(Sp. 2):140-152. Available in: https://pubmed.ncbi.nlm.nih.gov/34669285/
11. Neira Varillas MR, Donaires Toscano LF. Sífilis materna y complicaciones durante el embarazo. An. Fac. med. [Internet]. 2019 [cited 20/09/2024]; 80(1): 68-72. Available in: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1025-55832019000100013&lng=es
12. Guzmán M, Vergara R, Salazar M, Vargas RS, Aguilera Álvaro, De Uribe D. Las pruebas VDRL falsas reactivas en el manejo de la sífilis Reacciones Falsas positivas en el embarazo. biomedica [Internet]. 1981 [cited 20/09/2024]; 1(3):117-23. Available in: https://revistabiomedica.org/index.php/biomedica/article/view/1791
13. Walker GJA. Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database of Systematic Reviews 2001, Issue 3. Art. No.: CD001143. DOI: 10.1002/14651858.CD001143
14. Tuddenham S, Ghanem KG. Management of Adult Syphilis: Key Questions to Inform the 2021 Centers for Disease Control and Prevention Sexually Transmitted Infections Treatment Guidelines. Clin Infect Dis. 2022 [cited 20/09/2024]; 74(Suppl_2):S127-S133. Available in: https://pubmed.ncbi.nlm.nih.gov/35416969/
15. Trinh T, Leal AF, Mello MB, et al. Syphilis management in pregnancy: a review of guideline recommendations from countries around the world. Sex Reprod Health Matters. 2019 [cited 20/09/2024]; 27(1):69-82. Available in: https://pubmed.ncbi.nlm.nih.gov/31884900/
16. Nurse-Findlay S, Taylor MM, Savage M, et al. Shortages of benzathine penicillin for prevention of mother-to-child transmission of syphilis: An evaluation from multi-country surveys and stakeholder interviews. PLoS Med. 2017 [cited 20/09/2024]; 14(12):e1002473. Available in: https://pubmed.ncbi.nlm.nih.gov/29281619/
17. Méndez Valdés A. Sífilis Secundaria Durante el Embarazo: Importancia del Control Prenatal. Rev Méd Cient [Internet]. 2014 [cited 20/09/2024]; 26(2). Available in: https://www.revistamedicocientifica.org/index.php/rmc/article/view/381
18. Sidana R, Mangala HC, Murugesh SB, Ravindra K. Prozone phenomenon in secondary syphilis. Indian J Sex Transm Dis. 2011;32(1):47-9. DOI: 10.4103/0253-7184.81256.
19. Camacho-Montaño AM, Niño-Alba R, Páez-Castellanos E. Congenital syphilis with hydrops fetalis: report of four cases in a general referral hospital in Bogota, Colombia between 2016- 2020. Rev Colomb Obstet Ginecol. 2021 [citado 20/09/2024]; 72(2):149-161. doi: 10.18597/rcog.3591. PMID: 34506702; PMCID: PMC8425360.
20. Azevedo Dantas L, Jerônimo Neves de Medeiros SH, Teixeira Alves G, Lopes Gabriel TR, Cassiano Nascimento A, Carvalho Leite de JB. Perfil epidemiológico de sífilis adquirida diagnosticada y notificada en hospital universitario materno infantil. Enferm. glob. [Internet]. 2017 [cited 20/09/2024]; 16(46):217-245. Available in: http://scielo.isciii.es/z10.6018/eglobal.16.2.229371
STATEMENT OF AUTHORSHIP
MDMG: Conceptualization, investigation, methodology, project administration, validation, writing of the original draft, review, editing.
LNO: Conceptualization, investigation, methodology, validation, writing of the original draft, review.
DLB: Conceptualization, investigation, methodology, validation, writing of the original draft, review.
EZT: Conceptualization, investigation, methodology, validation, writing of the original draft, review.
CDBM: Conceptualization, investigation, methodology, validation, writing of the original draft, review.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
FUNDING SOURCES
The authors declare that they did not receive funding for the development of this research.