CASE PRESENTATION
Clinical and histopathological correlation in a dermatosis considered the great imitator: a case study
Correlación clínica e histopatológica en dermatosis considerada la gran simuladora: a propósito de un caso
Regla Katileidy Zamora Leonard 1* ![]() , Arlis
Velázquez Sánchez
1
, Arlis
Velázquez Sánchez
1![]() , Yenisey Román
Manrique 1
, Yenisey Román
Manrique 1![]() , Diana Maité
Hernández Fernández 1
, Diana Maité
Hernández Fernández 1![]()
1 Faustino Pérez Provincial Clinical-Surgical-Teaching Hospital. Matanzas, Cuba.
* Corresponding author: katy940906@gmail.com
Received: 18/09/2025
Accepted: 30/12/2025
How to cite this article: Zamora-Leonard RK, Velázquez-Sánchez A, Román-Manrique Y, Hernández-Fernández DM. Clinical and histopathological correlation in a dermatosis considered the great imitator: a case study. MedEst. [Internet]. 2026 [cited access date]; 6:e459. Available in: https://revmedest.sld.cu/index.php/medest/article/view/459
ABSTRACT
Introduction: syphilis, considered a sexually transmitted infection, is caused by the bacterium Treponema pallidum. Its incidence has significantly decreased; however, "the great imitator" remains, and it is essential to maintain a diagnostic suspicion since, in addition to the usual clinical forms, infrequent manifestations or those that mimic other diseases may arise, complicating timely detection depending on the evolutionary stage of the disease.
Objective: to determine the correlation of histological studies with the clinical suspicion of the disease.
Case Presentation: although histopathological study is not listed as a criterion for defining the index case and consequently the diagnosis of the condition, sometimes the diverse morphology of the lesions warrants the use of skin biopsy to rule out other conditions. A 54-year-old male patient presented with general and cutaneous manifestations lasting several weeks. Complementary tests were indicated for diagnosis and to initiate subsequent management. Additionally, a skin biopsy was performed to evaluate other diagnostic possibilities. The histological result confirmed the clinical suspicion of syphilis, demonstrating the importance of histology in dermatological conditions.
Conclusions: the clinical manifestations of syphilis are challenging, and their recognition is crucial. Although histology is not considered a laboratory criterion for diagnosis, clinical suspicion and skin biopsy with characteristic results of this infection were key elements in the patient's care.
Keywords: Dermatosis; Secondary syphilis; Treponema pallidum
RESUMEN
Introducción: la sífilis, considerada de transmisión sexual, es causada por la bacteria Treponema Pallidum. Su incidencia ha decrecido de forma significativa, sin embargo, ¨la gran simuladora¨ permanece y es preciso mantener la sospecha diagnóstica ya que además de las formas clínicas habituales, pueden aparecer manifestaciones infrecuentes o que simulen otra enfermedad, que dificulten la detección oportuna, según la etapa evolutiva en que se encuentre la misma.
Objetivo: determinar la correlación de los estudios histológicos con la sospecha clínica de la enfermedad.
Presentación del caso: aunque el estudio histopatológico no está señalado como criterio para definir el caso índice y por consecuencia el diagnóstico de la entidad, en ocasiones, la morfología diversa de las lesiones determina que se contemple el uso de la biopsia cutánea, para descartar otras afecciones. Se presenta un paciente masculino, de 54 años, con manifestaciones generales y cutáneas de varias semanas de evolución. Se Indicaron complementarios para el diagnóstico e iniciar conducta a seguir. Además, se realizó biopsia de piel para evaluar otras posibilidades diagnósticas. El resultado histológico corroboró la sospecha clínica de Sífilis y quedó demostrada la importancia de la histología en las afecciones dermatológicas.
Conclusiones: las manifestaciones clínicas de la sífilis son un reto y su reconocimiento es crucial. Aunque la histología no se considera un criterio de laboratorio para el diagnóstico, la sospecha clínica y la biopsia cutánea con resultados característicos de esta infección fueron elementos clave en la atención del paciente.
Palabras Claves: Dermatosis; Secundarismo sifilítico; Treponema Pallidum
INTRODUCTION
Syphilis is a systemic infectious disease caused by the bacterium Treponema pallidum. Its primary route of transmission is sexual, although it can also occur vertically (transplacentally) from mother to fetus. The microorganism penetrates through mucous membranes or breaks in the skin, creating a primary lesion from which it spreads via the lymphatic system to the regional lymph nodes and subsequently disseminates hematogenously. (1,2)
Its incidence is higher in young adults (20 to 49 years); however, due to contemporary sexual practices, it can be observed in other age groups. Regarding the distribution by sex, numerous studies report a predominance in males. (3-6)
Understanding the evolutionary chronology of syphilis is essential to establish the clinical stage at the time of diagnosis. After a variable incubation period (between 10 and 90 days, with an average of 21), the disease progresses intermittently, alternating between phases of symptomatic activity and periods of latency. (1,4)
The primary stage is defined by the appearance of the syphilitic chancre: one or more painless ulcers, usually genital or extragenital, accompanied by regional lymphadenopathy and bacteremia, lasting up to five weeks. Approximately fifteen days after the appearance of the chancre, non-treponemal serology (VDRL) becomes reactive. This is followed by an early latency period, characterized by the absence of clinical symptoms, but with persistent serological reactivity, which lasts between one and six weeks. (1,2,4)
Secondary syphilis, as many authors have described it, "appears like a storm in a clear sky." This is due to the diverse morphology of the lesions and the involvement of various systems: systemic, cutaneous, mucosal, appendage, and visceral manifestations. The elevated number of treponemes in the blood, the high number of skin and mucous membrane lesions, the increased contagiousness, and the VDRL reactivity in 100 % of patients are distinctive characteristics of this stage. This is followed by the early latency period, lasting from one to one and a half years. Next comes late syphilis, which can persist for 10 years or more. This stage can be symptomatic or asymptomatic and occurs in 30 % to 40 % of patients, characterized by skin, cardiovascular, and neurological lesions. (1,2,4,5)
Regarding classification, syphilis is divided into congenital and acquired, and these are further subdivided into early and late, according to the duration of the infection. (1,4) This classification determines the appropriate management for each patient.
Although its origin is uncertain, different historical accounts place it in Asia or America, prior to Columbus's voyages, spreading to Europe through sailors involved in various wars. Evolutionary theory suggests the possibility that syphilis developed from yaws between 1500 and 3000 BC (2,4). The name "syphilis" is attributed to the poem by Girolamo Fracastoro. In 1530, he narrated the misfortunes of a shepherd named Syphilo who, punished by the god Apollo, suffered a repulsive disease. This infection is also known as lues, a term introduced by Jean Fennel in the 16th century, meaning plague or pestilence in Latin (4,6,7). From the beginning of the 16th century, it was considered a scourge of humanity, remembered as the epidemic that afflicted 15 % of the European population at that time. (4)
During the 20th century, major scientific advances related to this condition occurred. In 1941, non-treponemal tests began to be used as a diagnostic tool, and two years later, penicillin was introduced as a treatment for the disease. (4,8) With the advent of immunofluorescence techniques, the FTA-ABS test began to be used as a specific test in 1962, and subsequently, in the 1990s, PCR studies were developed. Towards the end of the century, the complete sequencing of the Treponema pallidum genome was achieved. (7,8)
The parameters for diagnosis are: epidemiology, clinical stages, and treponemal or non-treponemal tests. Laboratory criteria must always be present to report a case and prescribe treatment.
Early detection of syphilis presents a diagnostic challenge due to its remarkable clinical pleomorphism, which frequently mimics other dermatological and infectious conditions. For dermatologists, timely recognition is a critical professional responsibility, not only because of its implications for individual patient management, but also because of its alignment with the public health objectives established in the National Strategic Plan for the Prevention and Control of STIs and HIV/AIDS. An accurate clinical suspicion is the fundamental starting point for initiating appropriate case management, investigating sexual contacts, and implementing interventions in exposed populations, thereby interrupting the chain of transmission.
In this context, this case is presented with the aim of determining the correlation between the histological findings and the clinical suspicion of the disease.
CLINICAL CASE
A 54-year-old male patient with no significant past medical history presented with a single lesion on his lower lip that appeared two weeks prior to the consultation. Five days later, multiple additional lesions suddenly appeared on his face and trunk. During this initial evaluation, given the clinical suspicion of a sexually transmitted infection (STI), serological tests were ordered (HIV, VDRL, hepatitis B surface antigen, and hepatitis C antibodies).
The patient returned to the institution two weeks later, reporting that he had not undergone the requested additional tests. At this second visit, he reported the onset of general constitutional symptoms, including loss of appetite, asthenia, malaise, and fever. He also described changes in the size and morphology of the pre-existing skin lesions. There was no documented history of drug allergies or recent exposure to known substances or allergens.
Cutaneous findings:
· Erythematous lesions, some reddish-purple, with an infiltrated and nodular appearance (Fig. 1).
· Multiple papules of varying size, shape, and number.
· Formation of plaques by the confluence of several lesions.
· Surface covered with dry, whitish, easily detachable, lamellar scales (Fig. 2).
· Generalized distribution, predominantly in the proximal regions of the upper and lower extremities, trunk, and face. Facial involvement gave a "leonine facies" appearance.
Neurodermatological examination: Negative for sensory or motor abnormalities.

Fig. 1: erythematous lesions, some reddish-purple in color, with an infiltrated and nodular appearance.

Fig. 2: erythematous papules, some reddish-purple, with an infiltrated and nodular appearance, with the presence of scales.
Additional Tests Ordered
1) Serology:
· HIV: Non-reactive.
· Hepatitis B (HBsAg): Non-reactive.
· Hepatitis C (anti-HCV antibodies): Non-reactive.
· VDRL: Not performed (due to logistical reasons beyond the patient's control).
2) Skin Biopsy:
· Site: Lesion on the dorsal region.
· Histopathological Report: "Superficial and deep nodular dermatitis, with a tuberculoid granulomatous pattern, abundant plasma cells in the inflammatory infiltrate, and marked endothelial cell hyperplasia. Epidermis preserved" (Fig. 3).
· Anatomopathological Conclusion: Compatible with secondary or tertiary syphilis
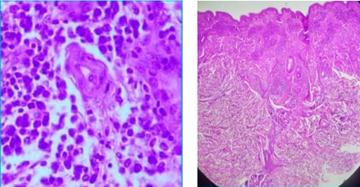
Fig. 3: Histological image compatible with secondary or tertiary syphilis.
To conclude and diagnose an index case of syphilis, the laboratory criterion (VDRL) is mandatory. This case never yielded the VDRL result because, for reasons beyond the patient's control, it could not be performed. With the histological result, the patient was referred to their local health center, after prior coordination with the dermatologist there. They were evaluated in the STI clinic, since this condition is reported, managed, and followed up in primary healthcare.
A referral was received for the case, which was treated with a single dose of 2.4 million units of benzathine penicillin. An epidemiological survey was conducted, and the patient is currently under serological follow-up.
DISCUSSION
This case illustrates an atypical, nodular-granulomatous presentation of secondary syphilis in a patient, in whom the inability to obtain immediate serological confirmation (VDRL) highlights the crucial value of the clinicopathological correlation in guiding timely therapeutic management.
Its importance to the scientific literature lies in reinforcing the role of skin biopsy as a critical diagnostic tool in contexts of high clinical suspicion when standard serological tests are unavailable or the clinical presentation deviates from classic manifestations—a scenario not uncommon in settings with logistical limitations or in rare presentations of the disease.
The clinical presentation of the patient presented, characterized by infiltrated papules and plaques with a generalized distribution and facial involvement ("leonine facies"), differs from the diffuse maculopapular forms typically described in secondary syphilis. This nodular and infiltrative morphology, although unusual, has been documented in case series and isolated reports, which emphasize its potential for confusion with other granulomatous or neoplastic entities. For example, Fernández Camporro et al. (8) and Rysgaard et al. (10) describe granulomatous histological patterns in nodular secondary syphilis, highlighting the presence of a dense infiltrate with plasma cells and vasculitis as key findings, which coincides with the authors' observations (tuberculoid granulomatous infiltrate, abundant plasma cells, and endothelial hyperplasia).
Similarly, Díaz Lobo et al. (5) and Merenzon et al. (7) report atypical presentations (neurosyphilis, ocular syphilis, ulcerated or desquamative lesions on fingertips) that were initially mistaken for other pathologies, underscoring the "great imitator" nature of syphilis and the need to maintain a high index of suspicion.
Regarding the therapeutic approach, the decision to initiate empirical treatment with benzathine penicillin (2.4 million units, single dose) based on strong clinical suspicion and histopathological support, before serological confirmation, aligns with public health recommendations for the control of sexually transmitted infections.
This action, followed by referral to the specialized STI clinic in primary care for notification, contact tracing, and serological follow-up, reflects comprehensive and timely management. The literature supports this approach in contexts of high clinical probability, where delays in treatment can increase transmissibility and the risk of complications. The National Strategic Plan for the Prevention and Control of STIs (Cuba, 2023) emphasizes the importance of clinical suspicion and rapid management to interrupt the chain of transmission, a principle that was successfully applied in this case.
The differential diagnoses considered (leprosy, sarcoidosis, cutaneous T-cell lymphomas, arboviral infections) were ruled out through a combination of clinical presentation, neurodermatological examination (no sensorimotor abnormalities), and the specific histological pattern (non-caseating granulomas with abundant plasma cells and vasculitis). Although histology alone is not pathognomonic, the aforementioned triad, in a suggestive epidemiological and clinical context, significantly increases the diagnostic probability of syphilis, as several authors concur. (9,11)
The main limitation is the initial absence of the VDRL test, the standard laboratory criterion for definitive confirmation. However, this very fact reinforces the central message of the case: in scenarios where serological confirmation is delayed or not feasible, a detailed histopathological evaluation can provide sufficient evidence to justify early therapeutic intervention and subsequent confirmation, thus fulfilling public health objectives.
CONCLUSIONS
This case underscores that cutaneous histopathology, while not a substitute for serology, is a crucial diagnostic pillar in atypical syphilis when standard confirmation is unavailable. The clinicopathological correlation allowed for timely empirical treatment with penicillin, aligned with public health objectives. It reaffirms the need to integrate all available tools when faced with unusual presentations of this “great imitator” and highlights the importance of a bold clinical approach to prioritize early intervention, avoiding delays that are detrimental to both the patient and transmission control.
BIBLIOGRAPHIC REFERENCES
1. Forrestel AK, Kovarik CL, Katz KA. Sexually acquired syphilis: historical aspects, microbiology, epidemiology, and clinical manifestations. J Am Acad Dermatol. 2020 Jan; 82(1):1-14. doi: 10.1016/j.jaad.2019.02.073.
2. Ghanem KG, Ram S, Rice PA. The modern epidemic of syphilis. N Engl J Med. 2020 Feb 27; 382(9):845-54. doi: 10.1056/NEJMra1901593.
3. Ministerio de Salud Pública (Cuba). Plan Estratégico nacional para la prevención y control de las ITS, el VIH y las hepatitis 2024-2028 (Bases normativas) [Internet]. La Habana: MINSAP; 2023 [cited 10/09/2025]. Available in: https://temas.sld.cu/vihsida/files/2016/12/Plan-Estrat%C3%A9gico-Nacional-ITS-VIH-hepatitis-2024-2028.pdf
4. Oreamuno YV, Boza SM. Sífilis la gran imitadora. Reporte de caso y revisión de la literatura. Odontoestomatología [Internet]. 2021 [cited 10/09/2025]. Available in: https://doi.org/10.22592/ode2021n37a7
5. Díaz Lobo ED, Piña RI, Murujosa A, Pollán J. Sífilis: formas de presentación poco frecuentes. Med Clin (Barc) [Internet]. 2023 [cited 10/09/2025]; 83(6):976-80. Available in: https://pubmed.ncbi.nlm.nih.gov/38117717/
6. Kantor IN. Sífilis en Argentina. Med Clin (Barc) [Internet]. 2023 [cited 10/09/2025]; 83(6):966-71. Available in: https://pubmed.ncbi.nlm.nih.gov/38117715/
7. Merenzon S, Barrio IA. Sífilis de presentación atípica. La gran simuladora. Med Clin (Barc) [Internet]. 2024 [cited 10/09/2025]; 84(5):1031. Available in: https://pubmed.ncbi.nlm.nih.gov/39399953/
8. Camporro A, Calzada González JM, Arcos González P, Rodríguez Díaz E. Sífilis secundaria granulomatosa: presentación de un caso sospechado a partir de los hallazgos histológicos. Actas Dermosifiliogr [Internet]. 2022 [cited 10/09/2025]; 113 Suppl 1:S26-8. Available in: https://pubmed.ncbi.nlm.nih.gov/36543465/
9. Wang X, Chen H, Sun J. Multiple nodules on the scalp as the only cutaneous symptom of secondary syphilis. Indian J Dermatol [Internet]. 2019 [cited 10/09/2025]; 58(10):e203-4. Available in: https://pubmed.ncbi.nlm.nih.gov/31236934/
10. Rysgaard C, Alexander E, Swick BL. Nodular secondary syphilis with associated granulomatous inflammation: case report and literature review. J Cutan Pathol [Internet]. 2014 [cited 10/09/2025]; 41(4):370-9. Available in: https://pubmed.ncbi.nlm.nih.gov/24447075/
11. Glatz M, Achermann Y, Kerl K, Bosshard PP, Cozzio A. Nodular secondary syphilis in a woman. BMJ Case Rep [Internet]. 2013 [cited 10/09/2025]. Available in: https://pubmed.ncbi.nlm.nih.gov/23661656/
12. Fitzpatrick T. Dermatología en Medicina General. 9ª ed. Buenos Aires: Editorial Médica Panamericana; 2024.
13. Arenas-Guzmán R. Dermatología. Atlas, Diagnóstico y tratamiento. 8ª ed. México: McGraw Hill Interamericana; 2024.
AUTHORSHIP STATEMENT
RKZL: Conceptualization, Data Curation, Formal Analysis, Research, Methodology, Drafting of the Original, Drafting of the Revision and Editing.
AVS: Conceptualization, Research, Drafting of the Original, Drafting of the Revision and Editing.
YRM: Research, Drafting of the Original, Drafting of the Revision and Editing.
DMHF: Research, Supervision, Drafting of the Original, Drafting of the Revision and Editing.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
FUNDING SOURCES
No external funding was received.